The Public Emergency Ended….Now What?

On April 10, 2023, President Biden signed a resolution ending both the COVID-19 National Emergency (ended April 10, 2023) and Public Health Emergency (ended May 11, 2023). With the expiration of the Public Health Emergency (PHE), health plans are no longer subject to federal requirements for coverage of COVID-19 testing, vaccinations, and treatments under the PHE.
Impact To Medical Benefits With The End Of PHE
Below is a summary of how COVID-19 coverage will be handled as of May 12, 2023:
| Coverage unchanged | Member cost share now applies |
|---|---|
The following benefits will continue after May 12, 2023, as they are required to be covered this way under the law. Members will continue to pay:
*Not applicable to grandfathered plans |
Benefits that were put in place during the PHE and provided at zero-cost share to the member will now be subject to member cost-share:
|
Impact To Key Timeframes With The End Of The National Emergency
The DOL and IRS have informally indicated that the May 11th Resolution does not affect the outbreak period’s end date of July 10, 2023, or the extensions that were previously granted. The
key deadlines extended during the outbreak period that will continue for a few more months include:
- HIPAA Special Enrollment Time Frames—The outbreak period extended the timeframe to request special enrollments under HIPAA. The May 11th Resolution did not impact those extensions. Though the timeframes vary by event, all extensions will expire no later than September 8, 2023. Plans sponsors should refer to their Plan Document or contact their W3 representative for specific questions related to HIPAA extensions.
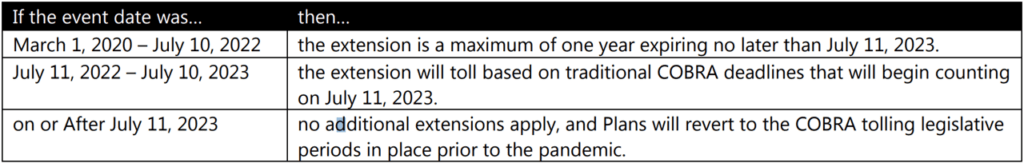
- COBRA Time Frames—The outbreak period extended the timeframe for qualified beneficiaries to elect COBRA coverage, make COBRA premium payments, and notify the Plan of a qualifying
event or disability determination. Timelines vary based on the event date, but are outlined here:
Claims, Appeals & External Review Process Time Frames: The outbreak period extended the timeframe to file a benefit claim, appeal an adverse benefit determination, or request an external review. Though the timeframes vary by situation, all extensions will expire no later than January 6, 2024. Plans sponsors should refer to their Plan Document or contact their W3 representative for specific questions related to these extensions.
Compliance
According to federal agencies, if changes are made to plan or coverage after the end of the PHE or National Emergency, plan sponsors and employers must clearly communicate these changes, including
any limitation on benefits, to participants and beneficiaries 60 days before they take effect. Additional resources on the ending of the COVID-19 emergency periods are available on the Department of
Labor’s Response to COVID-19 website, https://www.dol.gov/coronavirus.
This Compliance Bulletin is not intended to be exhaustive, nor should any discussion or opinions be construed as legal advice. Readers should contact legal counsel for legal advice.
